

Share
1st May 2018
05:00pm BST

 Talks of the importance of HIV awareness were spurred on by the passing of The Provision of Objective Sexual Education Bill at the Dáil just last week.
As it currently stands, there is no formal education for Irish students about sexually transmitted diseases.
In survey of 1,013 people in Ireland released by HIV Ireland in 2017, 93% of voters agreed that young people should be taught about HIV transmission during secondary school.
2018 sees HIV Ireland celebrate its 31st year offering support and information for people living with HIV and advocates on their behalf.
The organisation, which was previously known as the Dublin AIDS Alliance when it was established back in 1987, began tackling the disease when it was a very different prospect to what it is now.
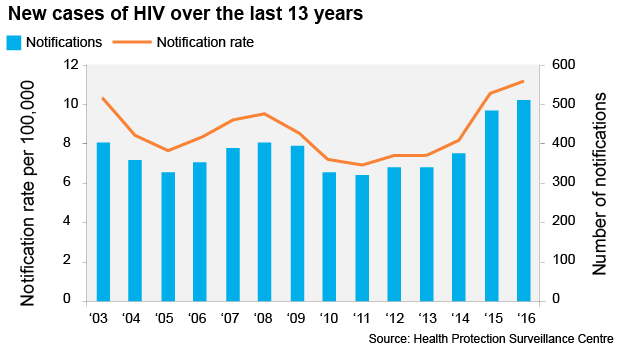
Executive Director Niall Mulligan of HIV Ireland explained to JOE that there are a number of factors as to why diagnoses figures are steadily growing each year.
"In essence, from our point of view – yes, the figures have been rising each year for a few reasons. Some of it is in terms of the HSE and HPSC and the way they conduct their testing service," he began.
[caption id="attachment_624559" align="aligncenter" width="771"]
Talks of the importance of HIV awareness were spurred on by the passing of The Provision of Objective Sexual Education Bill at the Dáil just last week.
As it currently stands, there is no formal education for Irish students about sexually transmitted diseases.
In survey of 1,013 people in Ireland released by HIV Ireland in 2017, 93% of voters agreed that young people should be taught about HIV transmission during secondary school.
2018 sees HIV Ireland celebrate its 31st year offering support and information for people living with HIV and advocates on their behalf.
The organisation, which was previously known as the Dublin AIDS Alliance when it was established back in 1987, began tackling the disease when it was a very different prospect to what it is now.
Executive Director Niall Mulligan of HIV Ireland explained to JOE that there are a number of factors as to why diagnoses figures are steadily growing each year.
"In essence, from our point of view – yes, the figures have been rising each year for a few reasons. Some of it is in terms of the HSE and HPSC and the way they conduct their testing service," he began.
[caption id="attachment_624559" align="aligncenter" width="771"] Credit: HPSC.ie[/caption]
"They're getting better at testing basically, showing quite a significant increase from years gone by.
“Another reason is that more and more people are coming into Ireland each year to study or work. If they have already been diagnosed with HIV in the country they are coming from, they still have to go through HIV testing – which is, in turn, adding to the figures.”
Mulligan went on to inform why this isn't necessarily a bad thing.
"Globally, some 30% of people living with HIV don't know they are. In Western Europe that figure decreases to about 15%.
"We actually look at this as a positive thing – it's good we're picking up it on more.
"As an individual, if you don't know you're living with HIV it can have a hugely negative impact on your body and it adds to onward transmission.
"Treatment in Ireland is free and it's excellent. Those who've contracted the disease through whatever way can quite easily get to a point of viral suppression, which means that although you still technically have HIV, the virus can no longer be detected in your body and you cannot spread it to others."
[caption id="attachment_624563" align="aligncenter" width="548"]
Credit: HPSC.ie[/caption]
"They're getting better at testing basically, showing quite a significant increase from years gone by.
“Another reason is that more and more people are coming into Ireland each year to study or work. If they have already been diagnosed with HIV in the country they are coming from, they still have to go through HIV testing – which is, in turn, adding to the figures.”
Mulligan went on to inform why this isn't necessarily a bad thing.
"Globally, some 30% of people living with HIV don't know they are. In Western Europe that figure decreases to about 15%.
"We actually look at this as a positive thing – it's good we're picking up it on more.
"As an individual, if you don't know you're living with HIV it can have a hugely negative impact on your body and it adds to onward transmission.
"Treatment in Ireland is free and it's excellent. Those who've contracted the disease through whatever way can quite easily get to a point of viral suppression, which means that although you still technically have HIV, the virus can no longer be detected in your body and you cannot spread it to others."
[caption id="attachment_624563" align="aligncenter" width="548"] Cred: HPSC.ie[/caption]
While assuring us that those who contract the disease in Ireland are well looked after physically, Mulligan has sensed a gaping hole in the market in terms of emotional wellbeing and counselling.
"There's a real gap here," he began.
"We have four counsellors in HIV Ireland, three volunteers, one paid, and they're at their max. In a recent survey we issued for people living with HIV, one of the things that jumped out was mental health.
"Out of the 190 people surveyed, 17% of those said they had considered suicide in wake of their diagnosis. They are pretty significant findings."
People have oftentimes suggested that the rise in figures has been spurred by readily available and online dating apps such as Grindr and Tinder.
Mulligan confirmed that the predominant route of HIV transmission they've noticed in HIV Ireland are men who have sex with men (MSM) – this group accounted for 51% of diagnoses in 2016 – but, according to recent figures, HIV Ireland can also confirm that this is not solely a man's issue.
Of the 508 cases reported in 2016, men claimed the vast majority of the diagnoses with 77% in comparison to the female diagnoses of 23%. But, when we look at the most recent stat, published in HPSC's week 16 report, we can see that during the week of 15/04/2018 - 21/04/2018, three men were diagnosed with the disease in comparison to two women.
For those diagnosed, treatment is the next protocol.
PrEP, the revolutionary drug that no longer equates a HIV diagnosis to a life-sentence, is a once-daily medication that, in combination with safer sex practices, has been proven to significantly reduce the risk of HIV infection.
PrEP is not currently available on the medical card in Ireland, but a generic one became available back in December, on Worlds AIDS Day.
Cred: HPSC.ie[/caption]
While assuring us that those who contract the disease in Ireland are well looked after physically, Mulligan has sensed a gaping hole in the market in terms of emotional wellbeing and counselling.
"There's a real gap here," he began.
"We have four counsellors in HIV Ireland, three volunteers, one paid, and they're at their max. In a recent survey we issued for people living with HIV, one of the things that jumped out was mental health.
"Out of the 190 people surveyed, 17% of those said they had considered suicide in wake of their diagnosis. They are pretty significant findings."
People have oftentimes suggested that the rise in figures has been spurred by readily available and online dating apps such as Grindr and Tinder.
Mulligan confirmed that the predominant route of HIV transmission they've noticed in HIV Ireland are men who have sex with men (MSM) – this group accounted for 51% of diagnoses in 2016 – but, according to recent figures, HIV Ireland can also confirm that this is not solely a man's issue.
Of the 508 cases reported in 2016, men claimed the vast majority of the diagnoses with 77% in comparison to the female diagnoses of 23%. But, when we look at the most recent stat, published in HPSC's week 16 report, we can see that during the week of 15/04/2018 - 21/04/2018, three men were diagnosed with the disease in comparison to two women.
For those diagnosed, treatment is the next protocol.
PrEP, the revolutionary drug that no longer equates a HIV diagnosis to a life-sentence, is a once-daily medication that, in combination with safer sex practices, has been proven to significantly reduce the risk of HIV infection.
PrEP is not currently available on the medical card in Ireland, but a generic one became available back in December, on Worlds AIDS Day.
 Teva Pharmaceuticals in Dundalk confirmed that the more affordable, generic version of the medication was to be made available in pharmacies in Ireland, on the back of a doctor’s prescription.
Teva’s PrEP, at time of writing, costs the patient about €100 a month, something that Director Mulligan still believes creates a barrier.
"Even at a reduced cost of approximately €100 per month it remains out of reach for many people who would benefit from PrEP.
"HIV Ireland encourages prevention over cure by the use of condoms, promoting safe sex, and urging intravenous drug users not to share injection equipment – but there's no doubt having PrEp on a medical card would break down financial barriers."
While PrEP is designed to be taken before engaging in intercourse, Mulligan also informed us of a drug that can be used in cases where the patient fears they may have contracted the disease following a sexual encounter.
Post Exposure Prophylaxis (PEP) has been around for quite a while and works similarly to a prolonged morning after pill. It must be taken within 72 hours of sexual intercourse and must be used for a month. However, not everyone can be prescribed it, it's essentially up to your GP's personal assessment.
Mulligan wants to see HIV discussed as part of the sexual health education curriculum, noting the topic isn’t broached in many schools.
"A lot of what we do is we're responding to people who present to us who are afraid that they may have contracted HIV, purely because they don't know how to tell or what's at risk if they do.
You're lucky if you've had good sex education here, it literally comes down to luck. Good sexual education in school is few and far between – if people don't know what risks they are putting themselves into, then we're not providing them with the tools to go forward and we are therefore putting them at risk ourselves.
"Myths based around HIV and other sexually transmitted diseases are still rampant among younger people which is very worrying. In another survey we did recently, it showed that 98% of people believed that HIV transmission should be taught in school."
Thankfully, getting tested for HIV couldn't be easier in this country.
https://twitter.com/HIV_Ireland/status/989807617710190592
You can check out your nearest free HIV and STI testing service centre with their locator map. Everywhere located on this map boasts a free testing service.
Otherwise, you can go to your GP or try out various clinics dotted around the country including Know Now, a rapid HIV testing for gay men.
With the rapid HIV testing service you will know your diagnosis within one minute. However, Mulligan did share that he believes there are "pros and cons" to that.
Most clinics have a callback system. This means that your results are guaranteed to get to you within two weeks.
Teva Pharmaceuticals in Dundalk confirmed that the more affordable, generic version of the medication was to be made available in pharmacies in Ireland, on the back of a doctor’s prescription.
Teva’s PrEP, at time of writing, costs the patient about €100 a month, something that Director Mulligan still believes creates a barrier.
"Even at a reduced cost of approximately €100 per month it remains out of reach for many people who would benefit from PrEP.
"HIV Ireland encourages prevention over cure by the use of condoms, promoting safe sex, and urging intravenous drug users not to share injection equipment – but there's no doubt having PrEp on a medical card would break down financial barriers."
While PrEP is designed to be taken before engaging in intercourse, Mulligan also informed us of a drug that can be used in cases where the patient fears they may have contracted the disease following a sexual encounter.
Post Exposure Prophylaxis (PEP) has been around for quite a while and works similarly to a prolonged morning after pill. It must be taken within 72 hours of sexual intercourse and must be used for a month. However, not everyone can be prescribed it, it's essentially up to your GP's personal assessment.
Mulligan wants to see HIV discussed as part of the sexual health education curriculum, noting the topic isn’t broached in many schools.
"A lot of what we do is we're responding to people who present to us who are afraid that they may have contracted HIV, purely because they don't know how to tell or what's at risk if they do.
You're lucky if you've had good sex education here, it literally comes down to luck. Good sexual education in school is few and far between – if people don't know what risks they are putting themselves into, then we're not providing them with the tools to go forward and we are therefore putting them at risk ourselves.
"Myths based around HIV and other sexually transmitted diseases are still rampant among younger people which is very worrying. In another survey we did recently, it showed that 98% of people believed that HIV transmission should be taught in school."
Thankfully, getting tested for HIV couldn't be easier in this country.
https://twitter.com/HIV_Ireland/status/989807617710190592
You can check out your nearest free HIV and STI testing service centre with their locator map. Everywhere located on this map boasts a free testing service.
Otherwise, you can go to your GP or try out various clinics dotted around the country including Know Now, a rapid HIV testing for gay men.
With the rapid HIV testing service you will know your diagnosis within one minute. However, Mulligan did share that he believes there are "pros and cons" to that.
Most clinics have a callback system. This means that your results are guaranteed to get to you within two weeks.Explore more on these topics: