

Share
9th May 2020
08:30am BST

 Saturday, 2 May was supposed to be Day Two of Joyce Kearney's hen weekend. Due to wed Gary in July, Joyce's friends had grand plans for a great weekend, but the wedding has now been postponed until July 2021. The silver lining is that Joyce and Gary got a Saturday slot for next year.
On Friday, with Gary making himself scarce elsewhere in their home, Joyce's friends organised a Zoom 'hen party' and had a ball. Gary did wonders in fashioning a sash for her and a few drinks and memories were shared online.
The next day, Joyce had her lie-in and headed into TUH for an overnight shift in the Radiology Department. "Sure enough," she says, "all the crew in work had arranged another little hen set-up for me in there. It was lovely."
Saturday, 2 May was supposed to be Day Two of Joyce Kearney's hen weekend. Due to wed Gary in July, Joyce's friends had grand plans for a great weekend, but the wedding has now been postponed until July 2021. The silver lining is that Joyce and Gary got a Saturday slot for next year.
On Friday, with Gary making himself scarce elsewhere in their home, Joyce's friends organised a Zoom 'hen party' and had a ball. Gary did wonders in fashioning a sash for her and a few drinks and memories were shared online.
The next day, Joyce had her lie-in and headed into TUH for an overnight shift in the Radiology Department. "Sure enough," she says, "all the crew in work had arranged another little hen set-up for me in there. It was lovely."
 "We would have been engaged 18 months when we got married, but it started to look doubtful a couple of months back," says Joyce.
"Then Gary was temporarily laid-off and we had to make a call on it. We prefer to say postponed rather than cancelled!
"It's funny how the wedding was the biggest thing in my life until this happened. Now, it doesn't matter. Life has a new perspective. We'll get there."
Every Covid-19 patient will go for an x-ray so the radiographers are as busy as they have ever been.
The hospitals may be eerily quiet in certain areas but the new Covid procedures - donning and doffing of Personal Protective Equipment (PPE) and deep cleans - mean everyone is kept going and it takes longer to get through the list of patients. A two-minute x-ray procedure is now followed by a 30-minute clean of the room.
The first few weeks of the pandemic reaching Irish shores, Joyce recalls, were tense.
"No-one knew what was coming and there was a real fear of the unknown," she says.
"It has been nine weeks since Ireland had its' first confirmed Covid-19 case and Joyce can sense a growing assuredness among her colleagues. They know what they are up against now.
Joyce hails from Wexford, while Gary is a Dub. Around the time of the government-advised lockdown, the couple sat down for a difficult chat.
"We would have been engaged 18 months when we got married, but it started to look doubtful a couple of months back," says Joyce.
"Then Gary was temporarily laid-off and we had to make a call on it. We prefer to say postponed rather than cancelled!
"It's funny how the wedding was the biggest thing in my life until this happened. Now, it doesn't matter. Life has a new perspective. We'll get there."
Every Covid-19 patient will go for an x-ray so the radiographers are as busy as they have ever been.
The hospitals may be eerily quiet in certain areas but the new Covid procedures - donning and doffing of Personal Protective Equipment (PPE) and deep cleans - mean everyone is kept going and it takes longer to get through the list of patients. A two-minute x-ray procedure is now followed by a 30-minute clean of the room.
The first few weeks of the pandemic reaching Irish shores, Joyce recalls, were tense.
"No-one knew what was coming and there was a real fear of the unknown," she says.
"It has been nine weeks since Ireland had its' first confirmed Covid-19 case and Joyce can sense a growing assuredness among her colleagues. They know what they are up against now.
Joyce hails from Wexford, while Gary is a Dub. Around the time of the government-advised lockdown, the couple sat down for a difficult chat.
"Gary had to make a decision - to stay with me and risk getting it [the virus] from me or going to stay with his parents. "And I've had to accept that I won't be back home any time soon. There are days when I've come home and cried; some difficult times. My family are in Wexford and it was my dad's 70th recently. I couldn't even go and wave from the end of their garden."The hospital provides an Employee Assistance Programme and the likes of guided meditation, workbooks and visits with psychologists have been made available. Colleagues have availed of these services but Joyce has been getting by and "touch wood", she hopes it continues. Gary chose to stay with Joyce and, she says, he has been the model partner. "I send him a text when I'm home. He will have the front door open and the shower on. I go straight up for a shower and wash my hair. Time is added onto everything. He has been very, very supportive and has everything cleaned and all my meals made. Who knows how long that will last?!" The curve has been flattened but the work goes on. For Joyce, her world is now work, home, Lidl and Circle K.
"I do feel that some of the praise we [frontline workers] are getting is unwarranted. We are doing our jobs and getting paid. Others are out of work and just trying to make ends meet. "People are saying we're heroes, but I'm only doing my job. I might not have signed up for a pandemic but I did sign up for this job, and it's a job I love. "I work with a good crew and I know that, when I'm going in, well do what is being asked of us and we'll have a bit of craic along the way."
 Brochan Delaney, porter. (Photo: Ian Boyle, JOE)[/caption]
"I was originally in the Meath Hospital and was a porter there for 14 years. I made the move out to Tallaght in 1998 so have been here since the start; 22 years."
Brochan 'Broch' Delaney is an institution at Tallaght University Hospital. 38 years a porter, the Finglas native makes the commute back and forth over the M50 for his shifts and can tell you stories as long as you have time in the day.
Broch and his wife are getting by as best they can in these straitened times but their situation is made even more difficult by minding his wife's 55-year-old sister with special needs. She would regularly attend St Michael's Day Centre but with that closed for the past two months, Broch and his wife are taking turns minding her. Added to that, he is "very conscious that I can bring it [the virus] home" and he is extra careful about showering and scrubbing after each shift.
Bringing 'it' home is commonly spoken of by the staff at hospitals and nursing homes across the country and with justification too.
There are just over 60 porters working at TUH, says Broch, and "15 or 16 have been out due to the virus". That means that one in four of the portering services at the hospital have either contracted Covid-19 or have self-isolated after suspecting they have symptoms.
Brochan Delaney, porter. (Photo: Ian Boyle, JOE)[/caption]
"I was originally in the Meath Hospital and was a porter there for 14 years. I made the move out to Tallaght in 1998 so have been here since the start; 22 years."
Brochan 'Broch' Delaney is an institution at Tallaght University Hospital. 38 years a porter, the Finglas native makes the commute back and forth over the M50 for his shifts and can tell you stories as long as you have time in the day.
Broch and his wife are getting by as best they can in these straitened times but their situation is made even more difficult by minding his wife's 55-year-old sister with special needs. She would regularly attend St Michael's Day Centre but with that closed for the past two months, Broch and his wife are taking turns minding her. Added to that, he is "very conscious that I can bring it [the virus] home" and he is extra careful about showering and scrubbing after each shift.
Bringing 'it' home is commonly spoken of by the staff at hospitals and nursing homes across the country and with justification too.
There are just over 60 porters working at TUH, says Broch, and "15 or 16 have been out due to the virus". That means that one in four of the portering services at the hospital have either contracted Covid-19 or have self-isolated after suspecting they have symptoms.
"It's a large number from our own department and the same for the household and cleaning departments. They are down to only three or four chefs. It's difficult but you have to keep going. It has to be done and we recognise that."For Broch, keeping going means extra shifts over consecutive days. He speaks with us on a sunny Saturday after coming off '12 days on the trot'. He has a day at home but is facing into seven more days of work in a row. Like so many of us, he tuned into An Taoiseach Leo Varadkar's address to the nation on Friday, 1 May and one major point leapt out - the pubs staying closed until August.
"The time-frame is a bit slow but we'll go with the flow. I usually love getting out and meeting people on my Saturdays. Going for a pint and backing a few horses. I do miss that. "At times, it gets in on you a bit but you can't allow it to for too long. You tell yourself that this is not going to last forever and that you're doing something good."
 Sinead Cleary, nurse. (Photo: Ian Boyle, JOE)[/caption]
Sinead Cleary is still doing a couple of women's health shifts in the hospital but is being redeployed to other departments and areas where she can help. Over the past weekend, she was working a 14-hour shift in the Adults Orthopaedics Department.
"We go wherever we are needed," she says. "I was in a non-Covid ward at the weekend. There were a lot of DIY injuries. One gentleman was hanging lights in his attic and fell through the ceiling."
Sinead's team, who all look after women's health, is a compact but efficient unit of eight. Three team members are currently out.
Sinead Cleary, nurse. (Photo: Ian Boyle, JOE)[/caption]
Sinead Cleary is still doing a couple of women's health shifts in the hospital but is being redeployed to other departments and areas where she can help. Over the past weekend, she was working a 14-hour shift in the Adults Orthopaedics Department.
"We go wherever we are needed," she says. "I was in a non-Covid ward at the weekend. There were a lot of DIY injuries. One gentleman was hanging lights in his attic and fell through the ceiling."
Sinead's team, who all look after women's health, is a compact but efficient unit of eight. Three team members are currently out.
"At the beginning, in the early weeks, that was when staff were starting to get sick and there were lots of patients coming in. When you have a small group, having two or three out can decimate you. The student nurses are coming in now, though, so that has made a big difference. "Some colleagues have been coming back in after getting sick, and recovering. I suppose the thought process is, 'If we don't go back and one of us get sick, who will look after us?' We don't want to leave our workmates on their own."Despite being down critical staff members, there is no deluge of patients coming in for checks. While that may sound like a relief, Sinead does have some valid concerns.
"All cervical check screenings have been suspended. Every woman who was due to have their smear test can't have it. Those women have had a run of it as it is. It would be great if we can get that up and running again, soon. If it goes any longer and people don't re-engage, we'll have other problems to deal with."Sinead and her husband, Brendan, have two children (aged six and 10) and he is working from home. Homework is being done on evenings and at the weekend but RTE's School Hub, she says, has been a blessing. Her father-in-law had a quadruple bypass not so long ago, so they are helping out by getting his shopping and dropping it over. Like Joyce and Broch, Sinead's first port of call is a long shower after she gets home. It can be tough at times, she says, but she is steeled by "a sense that we're all in this together". Her family and the work are keeping Sinead Cleary going. She gets calls from General Practitioners about them not being able to take smears of their patients and she wishes she had an answer on when that can get going again. She worries, too, about a second Covid-19 wave later in the year and knows now that it is best practice not to plan too far ahead.
"The patients understand and everyone has been great when they have called up. At the end of each phone call, you'll now get them asking after you - 'Now, how are you?' 'Are you okay?' 'Are you staying safe?' "That means an awful lot."
 Dr Brendan O'Daly, consultant orthopaedic surgeon. (Photo: Ian Boyle, JOE)[/caption]
Dealing with orthopaedics and trauma at TUH, surgeon Brendan Daly says surgical activities are down by around 50% but that weekends are just as busy as ever.
Dr Brendan O'Daly, consultant orthopaedic surgeon. (Photo: Ian Boyle, JOE)[/caption]
Dealing with orthopaedics and trauma at TUH, surgeon Brendan Daly says surgical activities are down by around 50% but that weekends are just as busy as ever.
"We are seeing a number of late presentations and that is worrying. People have held off on coming into us because they anticipate they are at risk of contracting Covid-19." "There was a study published in February, it was a major trauma audit. They checked the origins of cases seen in hospitals and what they found was that 50% of major trauma was incurred at home. That's falling over carpets or the end of the bed, falling off ladders, people doing DIY that they wouldn't normally do, cleaning out the shed and standing on a rusty nail. The patients that are coming in really are in need of the care."There are still a few severe industrial accidents to deal with but every patient, no matter where they were injured, has to go through Covid-19 procedures to stop the potential spread of transmission. The slow-down in patients coming in for elective procedures, such as knee and hip replacements, does not mean that waiting lists have been miraculously cleared. Brendan's other concern is that those lists will lengthen when hospitals want to get to full swing. It is now taking longer to see each patient, due to new Covid-19 procedures, so that may slow up the rate of surgeries he and his colleagues can get through each day. Away from work, Brendan and his wife are looking after their two-year-old son, who is not able to get to his regular childminder at present.
"I'm still going in for work and my wife is trying to work from home. You do have that fear, too, that you will contract Covid-19 and have to completely self-isolate. I'm the one who is most exposed to that. It has been challenging. It sounds like I am trying to play the violin there, but I'm not. That's the new reality for so many."The biggest surprise of the Covid-19 pandemic, says Brendan, has been seeing big sections of the hospital almost empty. "We are usually between 90% to full capacity year-round. But because of Covid there have been almost no non-Covid patients in so many parts. What was unexpected was such a dramatic reduction in non-presentations at hospitals." Before we finish up, Brendan wants to get in some thanks to other workers that are making life more bearable for those in the hospitals.
"Medical staff are hugely indebted to the people that are working away and doing vital services on the frontlines. Whether that's in the supermarkets, providing free coffees in petrol stations or hot meals for staff here at the weekend, it all makes a difference."If there can be three takeaways from the staff at Tallaght University Hospital, let them be:
 Members of the Household Cleaning Department[/caption]
[caption id="attachment_697361" align="aligncenter" width="1471"]
Members of the Household Cleaning Department[/caption]
[caption id="attachment_697361" align="aligncenter" width="1471"] Chef Alan Murray[/caption]
[caption id="attachment_697362" align="alignnone" width="1487"]
Chef Alan Murray[/caption]
[caption id="attachment_697362" align="alignnone" width="1487"] Bernadette Burke.[/caption]
[caption id="attachment_697366" align="aligncenter" width="1469"]
Bernadette Burke.[/caption]
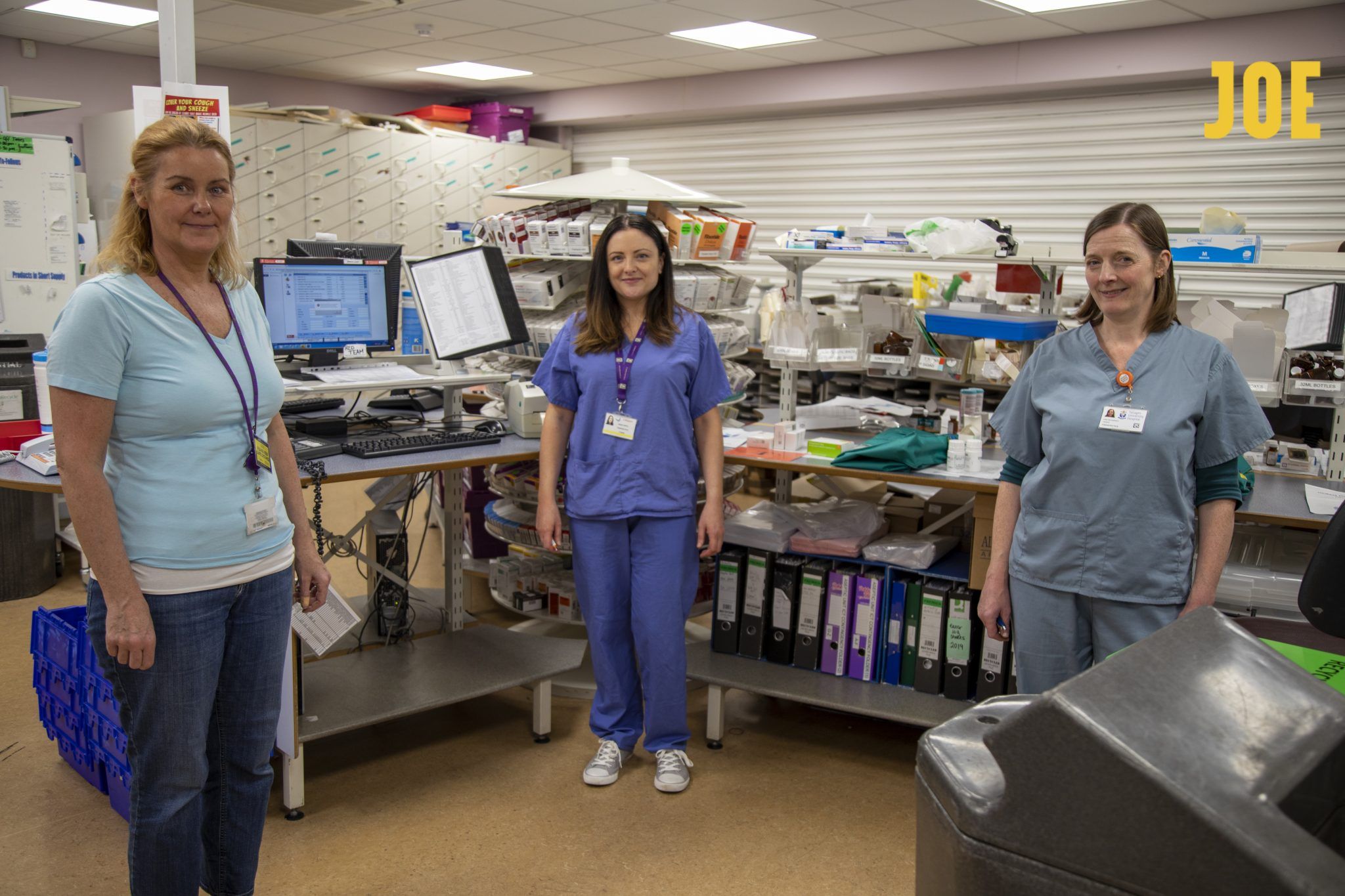
[caption id="attachment_697366" align="aligncenter" width="1469"] Diana Harte, senior pharmaceutical technician[/caption]
[caption id="attachment_697367" align="aligncenter" width="1365"]
Diana Harte, senior pharmaceutical technician[/caption]
[caption id="attachment_697367" align="aligncenter" width="1365"] Dr Emmet Browne[/caption]
Dr Emmet Browne[/caption]
 [caption id="attachment_697372" align="aligncenter" width="1365"]
[caption id="attachment_697372" align="aligncenter" width="1365"] Jenny Manoj, staff nurse[/caption]
[caption id="attachment_697373" align="aligncenter" width="1513"]
Jenny Manoj, staff nurse[/caption]
[caption id="attachment_697373" align="aligncenter" width="1513"] Shane Furlong, carpenter[/caption]
Shane Furlong, carpenter[/caption]Explore more on these topics: